Brain's frontal lobes affected by COVID-19 electrical activity disruptions
Brain Woes with COVID-19: EEG Reveals the Impact
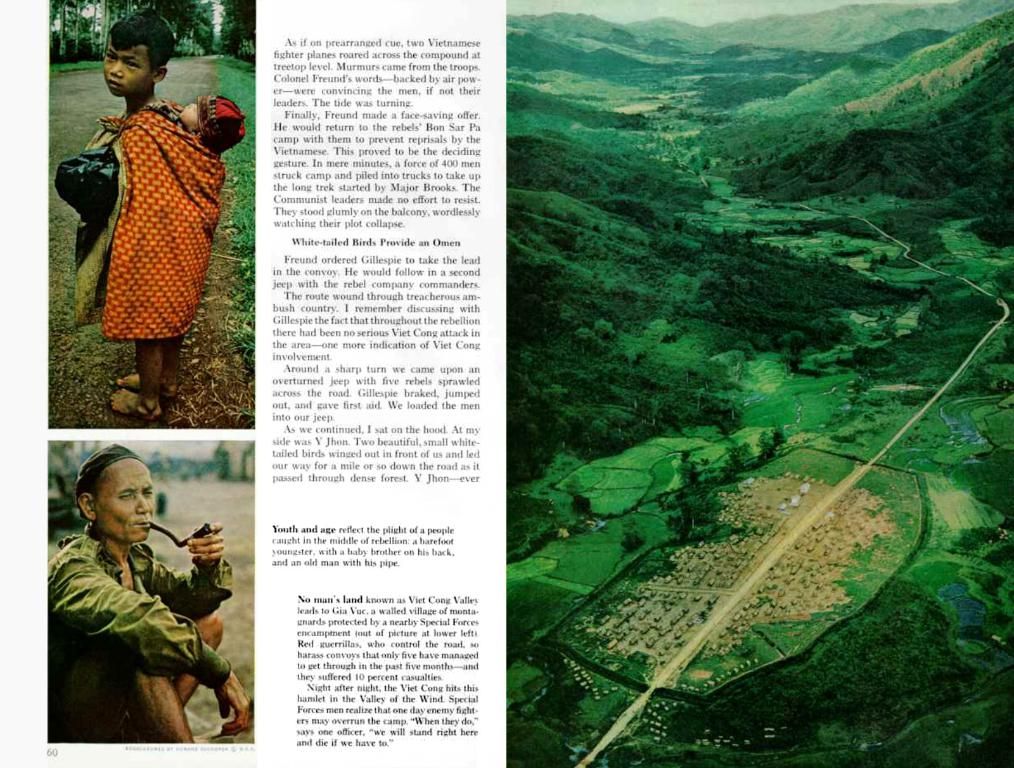
New research suggests that COVID-19 isn't just wrecking our lungs, but it's also messing with our noggins. A study, published in the journal Seizure: European Journal of Epilepsy, reveals estimated 15-25% of patients with severe COVID-19 could experience neurological symptoms like headaches, confusion, and strokes. To get to the root of this neurological puzzle, researchers analyzed EEG results from 617 patients, many of them exhibiting abnormalities in their brain activity, particularly in the frontal lobes.
As you'd expect, the virus may not be the sole culprit for these brain abnormalities. There are other factors, like chronic inflammation, low oxygen levels, and blood becoming extra sticky, playing a role. But what's most concerning is the link between the virus's entry point, the nose, and the frontal lobes, directly adjacent to it.
"We're thinking that the virus might be making a beeline for the brain through the nose, causing EEG abnormalities," explains Dr. Zulfi Haneef, one of the study's co-authors. "That's why we need to do more EEG tests to get a clearer picture of what's going on in the frontal lobe."
And the brain fog doesn't end with the acute phase. Many recovering COVID-19 patients report "brain fog," commonly known as long COVID. A recent cross-sectional study found that people who claim to have had the virus performed poorly on an online cognitive test, suggesting the infection may "age" brains by 10 years or more.
But don't panic just yet. The study didn't prove the infection caused long-term cognitive decline, but it did raise red flags. And with EEG abnormalities linked to COVID-19 neurological symptoms, experts like Dr. Haneef are more convinced than ever that brain-related complications could linger long past recovery. On the bright side, about 56.8% of those with follow-up EEG tests showed signs of improvement.
So, it seems COVID-19 is a multi-system invader, and unless we want to be brain-dead (literally or metaphorically), we better keep an eye on this RNA-douchebag. And if you start feeling like your head's been stuck in cotton candy for days, well, it might not just be a funny joke anymore. Best keep a neurodoc in your contacts, just in case.
[1] Systemic effects can include inflammation, low oxygen levels, blood becoming unusually sticky, and cardiac arrest.
[2] Study: MedRxiv. Accessed on 11/21/21. Link
[3] Science Media Centre. Accessed on 11/21/21. Link
[4] Case reports of neurological complications post-vaccination or COVID-19 infection are available. Some suggest a potential for exacerbating preexisting conditions or triggering new neurological issues.
- The ongoing research on COVID-19 has revealed that neurological symptoms, such as headaches, confusion, and strokes, could be experienced by 15-25% of patients with severe COVID-19.
- To better understand the impact of COVID-19 on the brain, electroencephalography (EEG) tests have been conducted and analyzed, showing abnormalities in brain activity, particularly in the frontal lobes.
- The link between COVID-19 and its potential entry point through the nose and the proximity of the frontal lobes is being examined, with concerns that the virus may be navigating towards the brain.
- Aside from the virus itself, factors such as chronic inflammation, low oxygen levels, and blood becoming excessively sticky could also contribute to the observed brain abnormalities.
- Beyond the acute phase of COVID-19, some patients continue to experience cognitive difficulties, often referred to as "brain fog," which may be long-lasting and indicative of a potential increase in health-and-wellness issues and neurological disorders like epilepsy seizures and other neurological-disorders.
- While more research is needed to confirm the long-term effects on the brain, the findings suggest that neurological complications from COVID-19 may persist beyond recovery, emphasizing the importance of monitoring and addressing these health concerns from a holistic health-and-wellness standpoint, including consideration for various medical-conditions and neurological-disorders.