Research insights on Vitamin D and joint discomfort: A look at the scientific findings
In a significant development, current evidence suggests a strong association between vitamin D deficiency and joint pain, particularly in diseases like rheumatoid arthritis (RA).
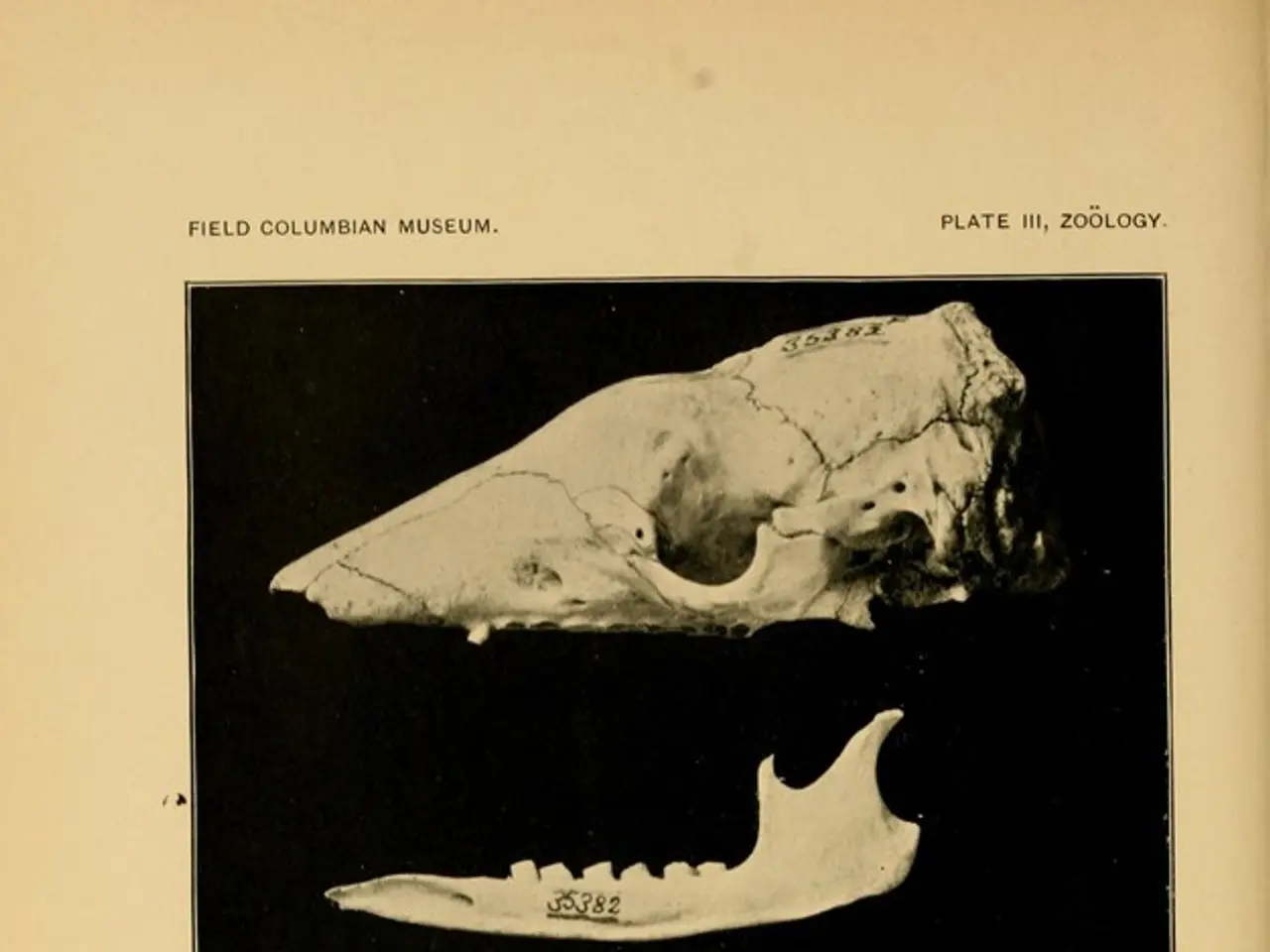
Vitamin D, a nutrient that helps regulate the amount of calcium in the body, plays a crucial role in bone health. It promotes calcium absorption and bone mineralization, making it vital for maintaining strong bones. Deficiency can lead to bone softening disorders such as osteomalacia in adults and rickets in children, which contribute to skeletal pain and weakness.
Beyond bone health, vitamin D influences immune modulation and inflammation. Given that rheumatoid arthritis is an autoimmune inflammatory disorder affecting joints, vitamin D deficiency is thought to exacerbate or increase susceptibility to RA. Indeed, vitamin D deficiency is listed among health complications related to RA.
Supplementation of vitamin D along with calcium has been shown to help prevent bone loss secondary to corticosteroid use in RA patients, suggesting a protective role in disease management. Although a direct causal link is complex to confirm, lower serum vitamin D levels have been observed in patients with joint pain and fragility fractures, hinting that deficiency may worsen joint symptoms or contribute to their development.
A review of studies from 2016 showed that people with RA had notably less vitamin D in their blood than people without RA, and they were more likely to have a vitamin D deficiency. Vitamin D supplementation is beneficial for the prevention of osteoporotic fractures in RA sufferers, who experience greater joint pain.
A Mediterranean diet, rich in probiotics, omega-3 polyunsaturated fatty acids, calcium, vitamin K, and antioxidants from brightly colored fruit, vegetables, nuts, and seeds, may also help relieve joint pain. Foods rich in vitamin D include oily fish, fortified milk, beef liver, egg yolks, mushrooms, and fortified breakfast cereals.
However, it's essential to note that while the evidence supports an association and potential benefit, it does not establish definitive causation. Further research continues to refine our understanding of vitamin D's role in rheumatoid arthritis.
Given the potential benefits, it's advisable for adults to aim to consume 15 micrograms (mcg) of vitamin D per day. However, too much vitamin D can cause toxicity, so it's best to consult a doctor or healthcare professional before taking supplements. Some people, such as vegetarians, older adults, and those with darker skin, may struggle to get enough vitamin D and may need supplements.
In conclusion, maintaining adequate vitamin D levels is considered beneficial in managing RA and preventing joint complications. A balanced diet and regular consultations with healthcare professionals can help ensure optimal vitamin D intake for overall health and joint wellbeing.
- A person with rheumatoid arthritis (RA) might experience more severe ulcerative and inflammatory symptoms as a result of vitamin D deficiencies.
- The immune system and inflammation are influenced by vitamin D, which makes it relevant to disorders such as psoriasis, colitis, and multiple sclerosis.
- A predictive relationship exists between low vitamin D levels and the onset or worsening of rheumatoid, psoriatic, or seasonal disorders.
- Nutrient-based therapies and treatments, including vitamin D supplements, can help manage chronic diseases like RA and psoriasis, among others.
- Rheumatoid arthritis patients, particularly those on corticosteroids, may benefit from vitamin D and calcium supplementation to prevent bone loss.
- Scientific studies suggest that people with RA are more likely to have low vitamin D levels in their blood compared to naive individuals, leading to a higher risk of deficiencies.
- The afflictive impact of vitamin D deficiency on affective medical-conditions like RA can be mitigated by a health-and-wellness oriented diet rich in vitamin D sources.
- People with rheumatoid arthritis and joint pain may find relief in the Mediterranean diet, which is abundant in vitamin D-rich foods like oily fish and fortified milk.
- While vitamin D supplementation is generally beneficial for RA patients, it's crucial to consult medical professionals to avoid potential toxicity and ensure proper dosage.
- Fitness and exercise, in addition to a balanced diet, are essential for maintaining the overall health, including vitamin D levels, which play a crucial role in joint health and wellbeing.
- Nutrient-rich diets, exercises, and treatments can contribute to improved joint health and reduced pain associated with chronic diseases like RA and psoriasis.
- Remaining conscious of vitamin D levels in the body becomes crucial for people suffering from neurological disorders like multiple sclerosis as they can also suffer from vitamin D deficiencies.
- Recent discoveries in the field of science reveal a link between vitamin D deficiency and rheumatoid arthritis, opening doors for future research into potential treatments.
- In the fitness-and-exercise and therapies-and-treatments realm, understanding the role of vitamin D in managing joint pain is essential for disease prevention and treatment.
- Various plant-based foods, such as mushrooms and fortified breakfast cereals, can be potential sources of vitamin D for vegetarians who may struggle to meet daily requirements through diet alone.