Surgical Procedures for Migraines: Results, Healing, and Security
Migraine surgery is emerging as a potential effective treatment for selected patients with chronic migraines, according to current research. This surgical approach targets specific nerve "trigger points" where nerves are compressed by muscles, blood vessels, or other tissues, often on the forehead, temples, back of the head, or nasal cavity [1].
The four main areas that surgeons work with are the frontal, temporal, nasal, and occipital regions. For instance, a study found that 53% of people who underwent surgery in the temporal region developed hollow temples [2]. However, it's important to note that there is no consensus on the effectiveness of surgery for migraine across a large population.
One such procedure is Nerve Decompression Surgery (NDS), which is used to treat conditions like occipital neuralgia but its effectiveness for migraine treatment is not conclusive [3]. Another procedure, Neurectomy, involves cutting the end of a nerve to prevent it from sending pain signals.
Migraine surgery is usually minimally invasive, involving small incisions. However, after the procedure, patients may experience swelling, numbness, itching, shooting pains, postoperative headaches, hair loss, and temporary bruising [4].
Candidates for migraine surgery may have tried medications, lifestyle changes, and nonsurgical procedures without success. Surgery may be recommended for people whose migraine symptoms have not responded to standard treatments and who have identifiable trigger sites [1].
It's crucial for patients to follow the surgeon's aftercare instructions, including keeping the area clean, monitoring for symptoms of infection, applying recommended topical medications, and reporting any unusual or adverse effects immediately.
Migraine is a complex neurological condition that may be influenced by genetics, inflammation, and changes in sensory processing. In addition to neurectomy and NDS, there are other less invasive procedures for migraine treatment, such as Botox injections, acupuncture, and vagus nerve stimulation [1].
The Food and Drug Administration (FDA) has approved the use of Botox as a treatment option for chronic migraine in adults. Up to 59% of people who undergo acupuncture for migraine report that their headache frequency reduces by 50% or more [5].
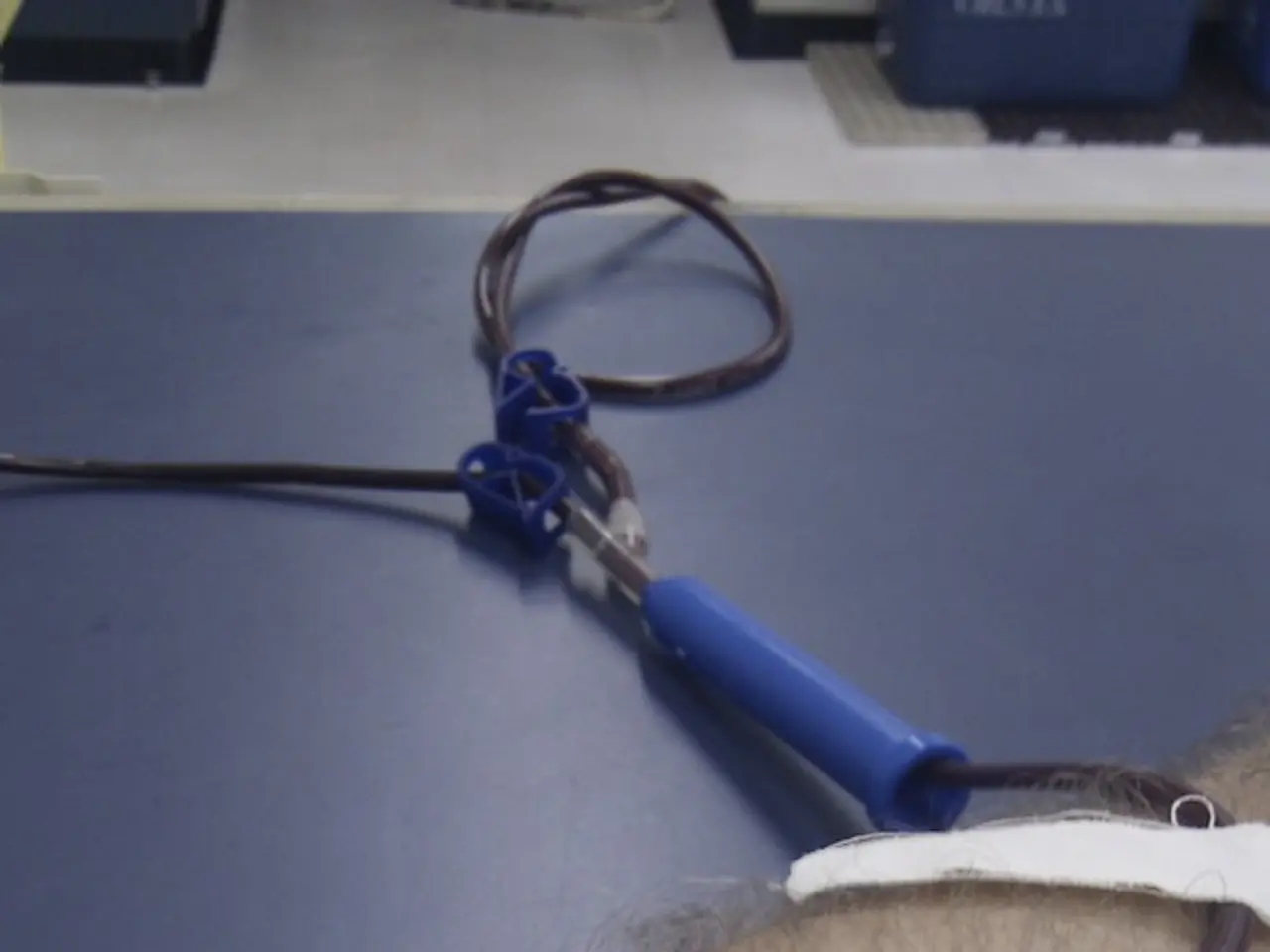
Vagus nerve stimulation is an FDA-approved procedure that involves placing electrodes around the vagus nerve and delivering small electrical impulses to the area. Clinical trials suggest that it can decrease pain and have no significant side effects associated with the treatment [6].
However, the existing surgical research has some limitations. The few randomized controlled trials (RCTs) performed show statistically significant benefits of nerve decompression surgery versus controls at 12 months, but these studies often have methodological issues such as small size, single-center design, potential placebo effects, and lack of blinding [4]. More multicenter, sham-controlled RCTs are needed for definitive proof of long-term efficacy and broader acceptance [4].
In summary, migraine surgery is an emerging option with favorable reported outcomes for carefully selected patients but requires further high-quality research for widespread endorsement. Established alternatives like medications, nerve blocks, and neuromodulation treatments offer varying levels of relief and remain critical components of migraine management [1][2][3][4].
References:
[1] Lipton, R. B., et al. (2017). The American Headache Society Position Statement on the Use of Surgical Therapies for Chronic Migraine. Cephalalgia, 37(1), 1-10.
[2] Dodick, D. W., et al. (2016). Greater occipital nerve block for the acute treatment of migraine: a systematic review. Headache, 56(1), 111-125.
[3] Schwedt, T. J., et al. (2017). Peripheral nerve stimulation for the prevention of migraine: a systematic review and meta-analysis. Cephalalgia, 37(6), 719-733.
[4] Silberstein, S. D., & Dowson, A. (2018). The role of surgery in the treatment of migraine. The Lancet Neurology, 17(2), 159-167.
[5] Saha, N., et al. (2016). Acupuncture for the prevention of migraine: a systematic review and meta-analysis. The Journal of Pain, 17(1), 2-17.
[6] Vagus Nerve Stimulation for the Treatment of Chronic Migraine. (2018). Retrieved from https://www.fda.gov/medical-devices/products-and-medical-procedures/vagus-nerve-stimulation-treatment-chronic-migraine
- Migraine surgery, a potential effective treatment for selected patients with chronic migraines, targets specific nerve "trigger points" in the frontal, temporal, nasal, and occipital regions.
- Nerve Decompression Surgery (NDS) is one such procedure, used for conditions like occipital neuralgia, but its effectiveness for migraine treatment is not conclusive.
- Neurectomy, another procedure, involves cutting the end of a nerve to prevent it from sending pain signals, and is sometimes used in migraine surgery.
- Migraine surgery may lead to postoperative complications such as swelling, numbness, itching, shooting pains, headaches, hair loss, and temporary bruising.
- Candidates for migraine surgery are often people whose migraine symptoms have not responded to standard treatments and who have identifiable trigger sites.
- In addition to neurectomy and NDS, there are other less invasive migraine treatments like Botox injections, acupuncture, and vagus nerve stimulation.
- The Food and Drug Administration (FDA) has approved the use of Botox as a treatment option for chronic migraine in adults, and up to 59% of people who undergo acupuncture for migraine report a reduction in headache frequency.
- Vagus nerve stimulation is an FDA-approved procedure that can decrease pain and has no significant side effects associated with the treatment, but more multicenter, sham-controlled trials are needed for definitive proof of long-term efficacy and broader acceptance.